Great article about Kinesio Tape and the Celtics from last year...
Kinesio Tape Working Wonders for Celtics
by Neil Keefe on Tue, Oct 20, 2009 at 4:22PM
If Kevin Garnett's right knee remains healthy this season, he can thank the unusual black tape wrapped around his leg for relieving all the pain,even if he doesn't know what the tape is or how it works. But then again, no one really knows how it works.
The tape is called Kinesio tape, and it has become a frequently-used pain reliever on the Celtics for both players and coaches.
"It just kind of relieves whatever is hurting," J.R. Giddens, who wears the tape on his right knee and back, told the Boston Herald. "It makes it feel better. I guess it’s the way it lays on the muscles, some pressure release or something."
"I don’t know what the hell it does, but it makes me feel better," Doc Rivers told the Herald. "It’s not just a tape, they put it on certain muscles .. I don’t know what the hell it does. Maybe it’s mental. I think a lot of teams are doing it and it’s been good. I know Kevin loves it."
How the tape works is still a mystery, but the wrapping technique became a hit during the 2008 Summer Olympics when Kinesio USA donated 50,000 rolls to the Games and athletes began wearing it.
Hasheem Thabeet, former UConn star and now member of the Memphis Grizzlies, used the tape on his shoulder throughout the season for the Huskies last year.
"There’s just not a ton of research on it," UConn basketball trainer James Doran told the Herald. "It’s not because when they do research it gets blown up, it’s just the research hasn’t been done. Kinesio tape originally started in Asia and it used to be like this secret taping that they used. It made its way to the New World and America and Europe have jumped on it. Again, when you try to find research on it, it’s just not there."
Dr. Joshua Brooks
Chiropractor, Fairfax VA
Wednesday, December 29, 2010
Thursday, December 23, 2010
Interferential Current Therapy for Musculoskeletal Pain
Effectiveness of Interferential Current Therapy in the Management of Musculoskeletal Pain: A Systematic Review and Meta-Analysisfrom Physical Therapy current issue by Fuentes, J. P., Armijo Olivo, S., Magee, D. J., Gross, D. P.
Background
Interferential current (IFC) is a common electrotherapeutic modality used to treat pain. Although IFC is widely used, the available information regarding its clinical efficacy is debatable.
Purpose
The aim of this systematic review and meta-analysis was to analyze the available information regarding the efficacy of IFC in the management of musculoskeletal pain.
Data Sources
Randomized controlled trials were obtained through a computerized search of bibliographic databases (ie, CINAHL, Cochrane Library, EMBASE, MEDLINE, PEDro, Scopus, and Web of Science) from 1950 to February 8, 2010.
Data Extraction
Two independent reviewers screened the abstracts found in the databases. Methodological quality was assessed using a compilation of items included in different scales related to rehabilitation research. The mean difference, with 95% confidence interval, was used to quantify the pooled effect. A chi-square test for heterogeneity was performed.
Data Synthesis
A total of 2,235 articles were found. Twenty studies fulfilled the inclusion criteria. Seven articles assessed the use of IFC on joint pain; 9 articles evaluated the use of IFC on muscle pain; 3 articles evaluated its use on soft tissue shoulder pain; and 1 article examined its use on postoperative pain. Three of the 20 studies were considered to be of high methodological quality, 14 studies were considered to be of moderate methodological quality, and 3 studies were considered to be of poor methodological quality. Fourteen studies were included in the meta-analysis.
Conclusion
Interferential current as a supplement to another intervention seems to be more effective for reducing pain than a control treatment at discharge and more effective than a placebo treatment at the 3-month follow-up. However, it is unknown whether the analgesic effect of IFC is superior to that of the concomitant interventions. Interferential current alone was not significantly better than placebo or other therapy at discharge or follow-up. Results must be considered with caution due to the low number of studies that used IFC alone. In addition, the heterogeneity across studies and methodological limitations prevent conclusive statements regarding analgesic efficacy.
Dr. Joshua Brooks
Chiropractor, Fairfax Va
Background
Interferential current (IFC) is a common electrotherapeutic modality used to treat pain. Although IFC is widely used, the available information regarding its clinical efficacy is debatable.
Purpose
The aim of this systematic review and meta-analysis was to analyze the available information regarding the efficacy of IFC in the management of musculoskeletal pain.
Data Sources
Randomized controlled trials were obtained through a computerized search of bibliographic databases (ie, CINAHL, Cochrane Library, EMBASE, MEDLINE, PEDro, Scopus, and Web of Science) from 1950 to February 8, 2010.
Data Extraction
Two independent reviewers screened the abstracts found in the databases. Methodological quality was assessed using a compilation of items included in different scales related to rehabilitation research. The mean difference, with 95% confidence interval, was used to quantify the pooled effect. A chi-square test for heterogeneity was performed.
Data Synthesis
A total of 2,235 articles were found. Twenty studies fulfilled the inclusion criteria. Seven articles assessed the use of IFC on joint pain; 9 articles evaluated the use of IFC on muscle pain; 3 articles evaluated its use on soft tissue shoulder pain; and 1 article examined its use on postoperative pain. Three of the 20 studies were considered to be of high methodological quality, 14 studies were considered to be of moderate methodological quality, and 3 studies were considered to be of poor methodological quality. Fourteen studies were included in the meta-analysis.
Conclusion
Interferential current as a supplement to another intervention seems to be more effective for reducing pain than a control treatment at discharge and more effective than a placebo treatment at the 3-month follow-up. However, it is unknown whether the analgesic effect of IFC is superior to that of the concomitant interventions. Interferential current alone was not significantly better than placebo or other therapy at discharge or follow-up. Results must be considered with caution due to the low number of studies that used IFC alone. In addition, the heterogeneity across studies and methodological limitations prevent conclusive statements regarding analgesic efficacy.
Dr. Joshua Brooks
Chiropractor, Fairfax Va
Thursday, August 19, 2010
Save Your Knees
Land on your toes, save your knees
August 10, 2010
Aggie player Paige Mintun goes for a layup and will be landing on those toes. (Wayne Tilcock/Davis Enterprise photo)
Anterior cruciate ligament injuries are a common and debilitating problem, especially for female athletes. A new study from UC Davis shows that changes in training can reduce shear forces on knee joints and could help cut the risk of developing ACL tears. The research was published online Aug. 3 in the Journal of Biomechanics.
"We focused on an easy intervention, and we were amazed that we could reduce shear load in 100 percent of the volunteers," said David Hawkins, professor of neurobiology, physiology and behavior at UC Davis. Hawkins conducted the study at the UC Davis Human Performance Laboratory with graduate student Casey Myers.
The anterior cruciate ligament lies in the middle of the knee and provides stability to the joint. Most ACL injuries do not involve a collision between players or a noticeably bad landing, said Sandy Simpson, UC Davis women's basketball coach.
"It almost always happens coming down from a rebound, catching a pass or on a jump-stop lay-up," Simpson said. "It doesn't have to be a big jump."
Hawkins and Myers worked with 14 female basketball players from UC Davis and local high schools. They fitted them with instruments and used digital cameras to measure their movements and muscle activity, and calculated the forces acting on their knee joints as they practiced a jump-stop movement, similar to a basketball drill.
First, they recorded the athletes making their normal movement. Then they instructed them in a modified technique: Jumping higher to land more steeply; landing on their toes; and bending their knees more deeply before taking off again.
After learning the new technique, all 14 volunteers were able to reduce the force passed up to the knee joint through the leg bone (the tibial shear force) by an average of 56 percent. At the same time, the athletes in the study actually jumped an inch higher than before, without losing speed.
Hawkins recommends warm-ups that exercise the knee and focusing on landing on the toes and balls of the feet. The study does not definitively prove that these techniques will reduce ACL injuries, Hawkins said: that would require a full clinical trial and follow-up. But the anecdotal evidence suggests that high tibial shear forces are associated with blown knees.
Hawkins and Myers shared their findings with Simpson and other UC Davis women’s basketball and soccer coaches, as well as with local youth soccer coaches.
Simpson said that the team had tried implementing some changes during last year's preseason, but had found it difficult to continue the focus once the full regular season began. In live play, athletes quickly slip back to learned habits and "muscle memory" takes over, he noted. More intensive off-court training and practice would be needed to change those habits, he said.
"We will be talking about this again this season," Simpson said. Implementing the techniques in youth leagues, while children are still learning how to move, might have the most impact, he said.
About UC Davis
For more than 100 years, UC Davis has engaged in teaching, research and public service that matter to California and transform the world. Located close to the state capital, UC Davis has 32,000 students, an annual research budget that exceeds $600 million, a comprehensive health system and 13 specialized research centers. The university offers interdisciplinary graduate study and more than 100 undergraduate majors in four colleges — Agricultural and Environmental Sciences, Biological Sciences, Engineering, and Letters and Science. It also houses six professional schools — Education, Law, Management, Medicine, Veterinary Medicine and the Betty Irene Moore School of Nursing.
Media contact(s):
•David Hawkins, Neurobiology, Physiology and Behavior, (530) 752-2748, dahawkins@ucdavis.edu
•Mike Robles, Intercollegiate Athletics, (530) 752-3680, merobles@ucdavis.edu
•Andy Fell, UC Davis News Service, (530) 752-4533, ahfell@ucdavis.edu
Dr. Joshua Brooks
Chiropractor Fairfax, VA 22031
Chiropractor Alexandria, VA 22304
August 10, 2010
Aggie player Paige Mintun goes for a layup and will be landing on those toes. (Wayne Tilcock/Davis Enterprise photo)
Anterior cruciate ligament injuries are a common and debilitating problem, especially for female athletes. A new study from UC Davis shows that changes in training can reduce shear forces on knee joints and could help cut the risk of developing ACL tears. The research was published online Aug. 3 in the Journal of Biomechanics.
"We focused on an easy intervention, and we were amazed that we could reduce shear load in 100 percent of the volunteers," said David Hawkins, professor of neurobiology, physiology and behavior at UC Davis. Hawkins conducted the study at the UC Davis Human Performance Laboratory with graduate student Casey Myers.
The anterior cruciate ligament lies in the middle of the knee and provides stability to the joint. Most ACL injuries do not involve a collision between players or a noticeably bad landing, said Sandy Simpson, UC Davis women's basketball coach.
"It almost always happens coming down from a rebound, catching a pass or on a jump-stop lay-up," Simpson said. "It doesn't have to be a big jump."
Hawkins and Myers worked with 14 female basketball players from UC Davis and local high schools. They fitted them with instruments and used digital cameras to measure their movements and muscle activity, and calculated the forces acting on their knee joints as they practiced a jump-stop movement, similar to a basketball drill.
First, they recorded the athletes making their normal movement. Then they instructed them in a modified technique: Jumping higher to land more steeply; landing on their toes; and bending their knees more deeply before taking off again.
After learning the new technique, all 14 volunteers were able to reduce the force passed up to the knee joint through the leg bone (the tibial shear force) by an average of 56 percent. At the same time, the athletes in the study actually jumped an inch higher than before, without losing speed.
Hawkins recommends warm-ups that exercise the knee and focusing on landing on the toes and balls of the feet. The study does not definitively prove that these techniques will reduce ACL injuries, Hawkins said: that would require a full clinical trial and follow-up. But the anecdotal evidence suggests that high tibial shear forces are associated with blown knees.
Hawkins and Myers shared their findings with Simpson and other UC Davis women’s basketball and soccer coaches, as well as with local youth soccer coaches.
Simpson said that the team had tried implementing some changes during last year's preseason, but had found it difficult to continue the focus once the full regular season began. In live play, athletes quickly slip back to learned habits and "muscle memory" takes over, he noted. More intensive off-court training and practice would be needed to change those habits, he said.
"We will be talking about this again this season," Simpson said. Implementing the techniques in youth leagues, while children are still learning how to move, might have the most impact, he said.
About UC Davis
For more than 100 years, UC Davis has engaged in teaching, research and public service that matter to California and transform the world. Located close to the state capital, UC Davis has 32,000 students, an annual research budget that exceeds $600 million, a comprehensive health system and 13 specialized research centers. The university offers interdisciplinary graduate study and more than 100 undergraduate majors in four colleges — Agricultural and Environmental Sciences, Biological Sciences, Engineering, and Letters and Science. It also houses six professional schools — Education, Law, Management, Medicine, Veterinary Medicine and the Betty Irene Moore School of Nursing.
Media contact(s):
•David Hawkins, Neurobiology, Physiology and Behavior, (530) 752-2748, dahawkins@ucdavis.edu
•Mike Robles, Intercollegiate Athletics, (530) 752-3680, merobles@ucdavis.edu
•Andy Fell, UC Davis News Service, (530) 752-4533, ahfell@ucdavis.edu
Dr. Joshua Brooks
Chiropractor Fairfax, VA 22031
Chiropractor Alexandria, VA 22304
Monday, July 26, 2010
Treatment for Back Pain in Fairfax, VA
A great article from ACA Today...
Does Back Pain Go Away on Its Own?
Eighty percent of people suffer from back pain at some point in their lives. Back pain is the second most common reason for visits to the doctor's office, outnumbered only by upper-respiratory infections. Most cases of back pain are mechanical or non-organic, i.e., not caused by serious conditions, such as inflammatory arthritis, infection, fracture, or cancer.
What Causes Back Pain?
The back is a complicated structure of bones, joints, ligaments, and muscles. You can sprain ligaments, strain muscles, rupture disks, and irritate joints, all of which can lead to back pain. While sports injuries or accidents can cause back pain, sometimes the simplest of movements-for example, picking up a pencil from the floor-can have painful results. In addition, arthritis, poor posture, obesity, and psychological stress can cause or complicate back pain. Back pain can also directly result from disease of the internal organs, such as kidney stones, kidney infections, blood clots, or bone loss.
Back injuries are a part of everyday life, and the spine is quite good at dealing with these often "pulled" muscles. These very minor injuries usually heal within 1 or 2 days. Some pain, however, continues. What makes some pain last longer is not entirely understood, but researchers suspect that the reasons may include stress, mood changes, and the fear of further injury that may prevent patients from being active. In addition, sometimes a painful injury or disease changes the way the pain signals are sent through the body, and, even after the problem has gone away or is inactive, the pain signals still reach the brain. It is as if the pain develops a memory that keeps being replayed.
Will Back Pain Go Away on Its Own?
Until recently, researchers believed that back pain will "heal" on its own. We have learned, however, that this is not true. A recent study showed that when back pain is not treated, it may go away temporarily but will most likely return. The study demonstrated that in more than 33% of the people who experience low-back pain, the pain lasts for more than 30 days. Only 9% of the people who had low-back pain for more than 30 days were pain free 5 years later.1
Another study looked at all of the available research on the natural history of low-back pain. The results showed that when it is ignored, back pain does not go away on its own.2 Those studies demonstrate that low-back pain continues to affect people for long periods after it first begins.
What Can I Do to Prevent Long-Term Back Pain?
If your back pain is not resolving quickly, visit your doctor of chiropractic. Your pain will often result from mechanical problems that your doctor of chiropractic can address. Many chiropractic patients with relatively long-lasting or recurring back pain feel improvement shortly after starting chiropractic treatment.3 The relief they feel after a month of treatment is often greater than after seeing a family physician.4
Chiropractic spinal manipulation is a safe and effective spine pain treatment. It reduces pain, decreases medication, rapidly advances physical therapy, and requires very few passive forms of treatment, such as bed rest.5
How Can I Prevent Back Pain?
Don't lift by bending over. Instead, bend your hips and knees and then squat to pick up the object. Keep your back straight, and hold the object close to your body.
Don't twist your body while lifting.
Push, rather than pull, when you must move heavy objects.
If you must sit for long periods, take frequent breaks and stretch.
Wear flat shoes or shoes with low heels.
Exercise regularly. An inactive lifestyle contributes to lower-back pain.
What Should I Tell My Doctor of Chiropractic?
Before any treatment session, tell your doctor of chiropractic if you experience any of the following:
Pain goes down your leg below your knee.
Your leg, foot, groin, or rectal area feels numb.
You have fever, nausea, vomiting, stomach ache, weakness, or sweating.
You lose bowel control.
Your pain is caused by an injury.
Your pain is so intense you can't move around.
Your pain doesn't seem to be getting better quickly.
--------------------------------------------------------------------------------
References
1.Hestbaek L, Leboeuf-Yde C, Engberg M, Lauritzen T, Bruun NH, Manniche C. The course of low-back pain in a general population. Results from a 5-year prospective study. J Manipulative Physiol Ther 2003 May;26(4):213-9.
2.Hestbaek L, Leboeuf-Yde C, Manniche C. Low-back pain: what is the long-term course? A review of studies of general patient populations. Eur Spine J 2003 Apr;12(2):149-65.
3.Stig LC, Nilsson O, Leboeuf-Yde C. Recovery pattern of patients treated with chiropractic spinal manipulative therapy for long-lasting or recurrent low back pain. J Manipulative Physiol Ther 2001 May;24(4):288-91.
4.Nyiendo J, Haas M, Goodwin P. Patient characteristics, practice activities, and one-month outcomes for chronic, recurrent low-back pain treated by chiropractors and family medicine physicians: a practice-based feasibility study. J Manipulative Physiol Ther 2000 May;23(4):239-45.
5.Time to recognize value of chiropractic care? Science and patient satisfaction surveys cite usefulness of spinal manipulation. Orthopedics Today February 2003;23(2):14-15.
Dr. Joshua Brooks,
Chiropractor Fairfax VA, Alexandria VA
Does Back Pain Go Away on Its Own?
Eighty percent of people suffer from back pain at some point in their lives. Back pain is the second most common reason for visits to the doctor's office, outnumbered only by upper-respiratory infections. Most cases of back pain are mechanical or non-organic, i.e., not caused by serious conditions, such as inflammatory arthritis, infection, fracture, or cancer.
What Causes Back Pain?
The back is a complicated structure of bones, joints, ligaments, and muscles. You can sprain ligaments, strain muscles, rupture disks, and irritate joints, all of which can lead to back pain. While sports injuries or accidents can cause back pain, sometimes the simplest of movements-for example, picking up a pencil from the floor-can have painful results. In addition, arthritis, poor posture, obesity, and psychological stress can cause or complicate back pain. Back pain can also directly result from disease of the internal organs, such as kidney stones, kidney infections, blood clots, or bone loss.
Back injuries are a part of everyday life, and the spine is quite good at dealing with these often "pulled" muscles. These very minor injuries usually heal within 1 or 2 days. Some pain, however, continues. What makes some pain last longer is not entirely understood, but researchers suspect that the reasons may include stress, mood changes, and the fear of further injury that may prevent patients from being active. In addition, sometimes a painful injury or disease changes the way the pain signals are sent through the body, and, even after the problem has gone away or is inactive, the pain signals still reach the brain. It is as if the pain develops a memory that keeps being replayed.
Will Back Pain Go Away on Its Own?
Until recently, researchers believed that back pain will "heal" on its own. We have learned, however, that this is not true. A recent study showed that when back pain is not treated, it may go away temporarily but will most likely return. The study demonstrated that in more than 33% of the people who experience low-back pain, the pain lasts for more than 30 days. Only 9% of the people who had low-back pain for more than 30 days were pain free 5 years later.1
Another study looked at all of the available research on the natural history of low-back pain. The results showed that when it is ignored, back pain does not go away on its own.2 Those studies demonstrate that low-back pain continues to affect people for long periods after it first begins.
What Can I Do to Prevent Long-Term Back Pain?
If your back pain is not resolving quickly, visit your doctor of chiropractic. Your pain will often result from mechanical problems that your doctor of chiropractic can address. Many chiropractic patients with relatively long-lasting or recurring back pain feel improvement shortly after starting chiropractic treatment.3 The relief they feel after a month of treatment is often greater than after seeing a family physician.4
Chiropractic spinal manipulation is a safe and effective spine pain treatment. It reduces pain, decreases medication, rapidly advances physical therapy, and requires very few passive forms of treatment, such as bed rest.5
How Can I Prevent Back Pain?
Don't lift by bending over. Instead, bend your hips and knees and then squat to pick up the object. Keep your back straight, and hold the object close to your body.
Don't twist your body while lifting.
Push, rather than pull, when you must move heavy objects.
If you must sit for long periods, take frequent breaks and stretch.
Wear flat shoes or shoes with low heels.
Exercise regularly. An inactive lifestyle contributes to lower-back pain.
What Should I Tell My Doctor of Chiropractic?
Before any treatment session, tell your doctor of chiropractic if you experience any of the following:
Pain goes down your leg below your knee.
Your leg, foot, groin, or rectal area feels numb.
You have fever, nausea, vomiting, stomach ache, weakness, or sweating.
You lose bowel control.
Your pain is caused by an injury.
Your pain is so intense you can't move around.
Your pain doesn't seem to be getting better quickly.
--------------------------------------------------------------------------------
References
1.Hestbaek L, Leboeuf-Yde C, Engberg M, Lauritzen T, Bruun NH, Manniche C. The course of low-back pain in a general population. Results from a 5-year prospective study. J Manipulative Physiol Ther 2003 May;26(4):213-9.
2.Hestbaek L, Leboeuf-Yde C, Manniche C. Low-back pain: what is the long-term course? A review of studies of general patient populations. Eur Spine J 2003 Apr;12(2):149-65.
3.Stig LC, Nilsson O, Leboeuf-Yde C. Recovery pattern of patients treated with chiropractic spinal manipulative therapy for long-lasting or recurrent low back pain. J Manipulative Physiol Ther 2001 May;24(4):288-91.
4.Nyiendo J, Haas M, Goodwin P. Patient characteristics, practice activities, and one-month outcomes for chronic, recurrent low-back pain treated by chiropractors and family medicine physicians: a practice-based feasibility study. J Manipulative Physiol Ther 2000 May;23(4):239-45.
5.Time to recognize value of chiropractic care? Science and patient satisfaction surveys cite usefulness of spinal manipulation. Orthopedics Today February 2003;23(2):14-15.
Dr. Joshua Brooks,
Chiropractor Fairfax VA, Alexandria VA
Wednesday, July 21, 2010
Electric Muscle Stimulation and Rehab
Effects of Neuromuscular Electrical Stimulation After Anterior Cruciate Ligament Reconstruction on Quadriceps Strength, Function, and Patient-Oriented Outcomes: A Systematic Reviewfrom Journal of Orthopaedic & Sports Physical Therapy - JOSPT Site-Wide RSSKyung-Min Kim, Ted Croy, Jay Hertel, Susan Saliba
STUDY DESIGN: Systematic literature review.
OBJECTIVE: To perform a systematic review of randomized controlled trials assessing the effects of neuromuscular electrical stimulation (NMES) on quadriceps strength, functional performance, and self-reported function after anterior cruciate ligament reconstruction.BACKGROUND: Conflicting evidence exists regarding the effectiveness of NMES following anterior cruciate ligament reconstruction.
METHODS: Searches were performed for randomized controlled trials using electronic databases from 1966 through October 2008. Methodological quality was assessed using the Physiotherapy Evidence Database Scale. Between-group effect sizes and 95% confidence intervals (CIs) were calculated.RESULTS: Eight randomized controlled trials were included. The average Physiotherapy Evidence Database Scale score was 4 out of possible maximum 10. The effect sizes for quadriceps strength measures (isometric or isokinetic torque) from 7 studies ranged from –0.74 to 3.81 at approximately 6 weeks postoperatively; 6 of 11 comparisons were statistically significant, with strength benefits favoring NMES treatment. The effect sizes for functional performance measures from 1 study ranged from 0.07 to 0.64 at 6 weeks postoperatively; none of 3 comparisons were statistically significant, and the effect sizes for self-reported function measures from 1 study were 0.66 and 0.72 at 12 to 16 weeks postoperatively; both comparisons were statistically significant, with benefits favoring NMES treatment.
CONCLUSION: NMES combined with exercise may be more effective in improving quadriceps strength than exercise alone, whereas its effect on functional performance and patient-oriented outcomes is inconclusive. Inconsistencies were noted in the NMES parameters and application of NMES. LEVEL OF EVIDENCE: Therapy, level 1a–.
Dr. Joshua Brooks
Chiropractor Fairfax, VA 22031
Chiropractor Alexandria, VA 22304
STUDY DESIGN: Systematic literature review.
OBJECTIVE: To perform a systematic review of randomized controlled trials assessing the effects of neuromuscular electrical stimulation (NMES) on quadriceps strength, functional performance, and self-reported function after anterior cruciate ligament reconstruction.BACKGROUND: Conflicting evidence exists regarding the effectiveness of NMES following anterior cruciate ligament reconstruction.
METHODS: Searches were performed for randomized controlled trials using electronic databases from 1966 through October 2008. Methodological quality was assessed using the Physiotherapy Evidence Database Scale. Between-group effect sizes and 95% confidence intervals (CIs) were calculated.RESULTS: Eight randomized controlled trials were included. The average Physiotherapy Evidence Database Scale score was 4 out of possible maximum 10. The effect sizes for quadriceps strength measures (isometric or isokinetic torque) from 7 studies ranged from –0.74 to 3.81 at approximately 6 weeks postoperatively; 6 of 11 comparisons were statistically significant, with strength benefits favoring NMES treatment. The effect sizes for functional performance measures from 1 study ranged from 0.07 to 0.64 at 6 weeks postoperatively; none of 3 comparisons were statistically significant, and the effect sizes for self-reported function measures from 1 study were 0.66 and 0.72 at 12 to 16 weeks postoperatively; both comparisons were statistically significant, with benefits favoring NMES treatment.
CONCLUSION: NMES combined with exercise may be more effective in improving quadriceps strength than exercise alone, whereas its effect on functional performance and patient-oriented outcomes is inconclusive. Inconsistencies were noted in the NMES parameters and application of NMES. LEVEL OF EVIDENCE: Therapy, level 1a–.
Dr. Joshua Brooks
Chiropractor Fairfax, VA 22031
Chiropractor Alexandria, VA 22304
Monday, July 19, 2010
Gait Biomechanics
Gait Biomechanics, Spatial and Temporal Characteristics, and the Energy Cost of Walking in Older Adults With Impaired Mobilityfrom Physical Therapy current issue by Wert, D. M., Brach, J., Perera, S., VanSwearingen, J. M.
Background
Abnormalities of gait and changes in posture during walking are more common in older adults than in young adults and may contribute to an increase in the energy expended for walking.
Objective
The objective of this study was to examine the contributions of abnormalities of gait biomechanics (hip extension, trunk flexion, and foot-floor angle at heel-strike) and gait characteristics (step width, stance time, and cadence) to the energy cost of walking in older adults with impaired mobility.
Design
A cross-sectional design was used.
Methods
Gait speed, step width, stance time, and cadence were derived during walking on an instrumented walkway. Trunk flexion, hip extension, and foot-floor angle at heel contact were assessed during overground walking. The energy cost of walking was determined from oxygen consumption data collected during treadmill walking. All measurements were collected at the participants' usual, self-selected walking speed.
Results
Fifty community-dwelling older adults with slow and variable gait participated. Hip extension, trunk flexion, and step width were factors related to the energy cost of walking. Hip extension, step width, and cadence were the only gait measures beyond age and gait speed that provided additional contributions to the variance of the energy cost, with mean R2 changes of .22, .12, and .07, respectively.
Limitations
Other factors not investigated in this study (interactions among variables, psychosocial factors, muscle strength [force-generating capacity], range of motion, body composition, and resting metabolic rate) may further explain the greater energy cost of walking in older adults with slow and variable gait.
Conclusions
Closer inspection of hip extension, step width, and cadence during physical therapy gait assessments may assist physical therapists in recognizing factors that contribute to the greater energy cost of walking in older adults.
Dr. Joshua Brooks,
Chiropractor Fairfax, VA 22031
Chiropractor Alexandria, VA 22304
Background
Abnormalities of gait and changes in posture during walking are more common in older adults than in young adults and may contribute to an increase in the energy expended for walking.
Objective
The objective of this study was to examine the contributions of abnormalities of gait biomechanics (hip extension, trunk flexion, and foot-floor angle at heel-strike) and gait characteristics (step width, stance time, and cadence) to the energy cost of walking in older adults with impaired mobility.
Design
A cross-sectional design was used.
Methods
Gait speed, step width, stance time, and cadence were derived during walking on an instrumented walkway. Trunk flexion, hip extension, and foot-floor angle at heel contact were assessed during overground walking. The energy cost of walking was determined from oxygen consumption data collected during treadmill walking. All measurements were collected at the participants' usual, self-selected walking speed.
Results
Fifty community-dwelling older adults with slow and variable gait participated. Hip extension, trunk flexion, and step width were factors related to the energy cost of walking. Hip extension, step width, and cadence were the only gait measures beyond age and gait speed that provided additional contributions to the variance of the energy cost, with mean R2 changes of .22, .12, and .07, respectively.
Limitations
Other factors not investigated in this study (interactions among variables, psychosocial factors, muscle strength [force-generating capacity], range of motion, body composition, and resting metabolic rate) may further explain the greater energy cost of walking in older adults with slow and variable gait.
Conclusions
Closer inspection of hip extension, step width, and cadence during physical therapy gait assessments may assist physical therapists in recognizing factors that contribute to the greater energy cost of walking in older adults.
Dr. Joshua Brooks,
Chiropractor Fairfax, VA 22031
Chiropractor Alexandria, VA 22304
Friday, May 21, 2010
Exercise to Reduce Pain
Aerobic Exercise Alters Analgesia and Neurotrophin-3 Synthesis in an Animal Model of Chronic Widespread Painfrom Physical Therapy current issue by Sharma, N. K., Ryals, J. M., Gajewski, B. J., Wright, D. E.
Background
Present literature and clinical practice provide strong support for the use of aerobic exercise in reducing pain and improving function for individuals with chronic musculoskeletal pain syndromes. However, the molecular basis for the positive actions of exercise remains poorly understood. Recent studies suggest that neurotrophin-3 (NT-3) may act in an analgesic fashion in various pain states.
Objective
The purpose of the present study was to examine the effects of moderate-intensity aerobic exercise on pain-like behavior and NT-3 in an animal model of widespread pain.
Design
This was a repeated-measures, observational cross-sectional study.
Methods
Forty female mice were injected with either normal (pH 7.2; n=20) or acidic (pH 4.0; n=20) saline in the gastrocnemius muscle to induce widespread hyperalgesia and exercised for 3 weeks. Cutaneous (von Frey monofilament) and muscular (forceps compression) mechanical sensitivity were assessed. Neurotrophin-3 was quantified in 2 hind-limb skeletal muscles for both messenger RNA (mRNA) and protein levels after exercise training. Data were analyzed with 2-factor analysis of variance for repeated measures (group x time).
Results
Moderate-intensity aerobic exercise reduced cutaneous and deep tissue hyperalgesia induced by acidic saline and stimulated NT-3 synthesis in skeletal muscle. The increase in NT-3 was more pronounced at the protein level compared with mRNA expression. In addition, the increase in NT-3 protein was significant in the gastrocnemius muscle but not in the soleus muscle, suggesting that exercise can preferentially target NT-3 synthesis in specific muscle types.
Limitations
Results are limited to animal models and cannot be generalized to chronic pain syndromes in humans.
Conclusions
This is the first study demonstrating the effect of exercise on deep tissue mechanical hyperalgesia in a rodent model of pain and providing a possible molecular basis for exercise training in reducing muscular pain.
Dr. Joshua Brooks
Chiropractor Fairfax VA 22031
Chiropractor Alexandria VA 22304
Background
Present literature and clinical practice provide strong support for the use of aerobic exercise in reducing pain and improving function for individuals with chronic musculoskeletal pain syndromes. However, the molecular basis for the positive actions of exercise remains poorly understood. Recent studies suggest that neurotrophin-3 (NT-3) may act in an analgesic fashion in various pain states.
Objective
The purpose of the present study was to examine the effects of moderate-intensity aerobic exercise on pain-like behavior and NT-3 in an animal model of widespread pain.
Design
This was a repeated-measures, observational cross-sectional study.
Methods
Forty female mice were injected with either normal (pH 7.2; n=20) or acidic (pH 4.0; n=20) saline in the gastrocnemius muscle to induce widespread hyperalgesia and exercised for 3 weeks. Cutaneous (von Frey monofilament) and muscular (forceps compression) mechanical sensitivity were assessed. Neurotrophin-3 was quantified in 2 hind-limb skeletal muscles for both messenger RNA (mRNA) and protein levels after exercise training. Data were analyzed with 2-factor analysis of variance for repeated measures (group x time).
Results
Moderate-intensity aerobic exercise reduced cutaneous and deep tissue hyperalgesia induced by acidic saline and stimulated NT-3 synthesis in skeletal muscle. The increase in NT-3 was more pronounced at the protein level compared with mRNA expression. In addition, the increase in NT-3 protein was significant in the gastrocnemius muscle but not in the soleus muscle, suggesting that exercise can preferentially target NT-3 synthesis in specific muscle types.
Limitations
Results are limited to animal models and cannot be generalized to chronic pain syndromes in humans.
Conclusions
This is the first study demonstrating the effect of exercise on deep tissue mechanical hyperalgesia in a rodent model of pain and providing a possible molecular basis for exercise training in reducing muscular pain.
Dr. Joshua Brooks
Chiropractor Fairfax VA 22031
Chiropractor Alexandria VA 22304
Friday, May 14, 2010
Knee Osteoarthritis
Moving to Maintain Function in Knee Osteoarthritis:
Evidence From the Osteoarthritis Initiative from Archives of Physical Medicine and Rehabilitation by Dorothy D. Dunlop, Pamela Semanik, Jing Song, Leena Sharma, Michael Nevitt, Rebecca Jackson, Jerry Mysiw, Rowland W. Chang, Osteoarthritis Initiative Investigators
Abstract: Dunlop DD, Semanik P, Song J, Sharma L, Nevitt M, Mysiw J, Chang RW, for the Osteoarthritis Initiative Investigators. Moving to maintain function in knee osteoarthritis: evidence from the Osteoarthritis Initiative.
Objectives: To investigate the association between baseline physical activity and 1-year functional performance in adults with knee osteoarthritis (OA).Design: Prospective cohort study of knee OA development and progression with 1-year follow-up.
Setting: Community.Participants: Osteoarthritis Initiative public data on adults with knee OA (n=2274; age, 45–79y) who participated in functional performance assessments (timed 20-m walk and chair stand test) at baseline and 1-year follow-up.Interventions: Not applicable.Main Outcome Measure: A good 1-year performance outcome (separately defined for walk time and chair stand measures) was improvement from baseline quintile or maintenance in the best quintile.
Results: Almost 2 in 5 persons with radiographic knee OA improved or maintained high performance at 1 year. Physical activity measured by the Physical Activity Scale for the Elderly (PASE) was significantly associated with good walk rate and chair stand outcomes (odds ratio per 40 units PASE [95% confidence interval]=1.13 [1.13, 1.17] and 1.10 [1.05, 1.15], respectively), as were participation in sports/recreational activities (1.45 [1.23, 1.71] and 1.29 [1.09, 1.51], respectively) and lifestyle activities (1.11 [1.06, 1.16] and 1.09 [1.04, 1.14], respectively). An independent protective relationship for these physical activity measures approached significance after adjusting for sociodemographic and health factors. Older adults reported the least baseline physical activity and least frequent good 1-year outcomes.
Conclusions: These findings support public health recommendations to be physically active in order to preserve function for persons with knee OA. Physical activity messages should specifically target older adults whose low activity levels may jeopardize their ability to maintain functional performance.
Dr. Joshua Brooks
Chiropractor Fairfax VA 22031
Evidence From the Osteoarthritis Initiative from Archives of Physical Medicine and Rehabilitation by Dorothy D. Dunlop, Pamela Semanik, Jing Song, Leena Sharma, Michael Nevitt, Rebecca Jackson, Jerry Mysiw, Rowland W. Chang, Osteoarthritis Initiative Investigators
Abstract: Dunlop DD, Semanik P, Song J, Sharma L, Nevitt M, Mysiw J, Chang RW, for the Osteoarthritis Initiative Investigators. Moving to maintain function in knee osteoarthritis: evidence from the Osteoarthritis Initiative.
Objectives: To investigate the association between baseline physical activity and 1-year functional performance in adults with knee osteoarthritis (OA).Design: Prospective cohort study of knee OA development and progression with 1-year follow-up.
Setting: Community.Participants: Osteoarthritis Initiative public data on adults with knee OA (n=2274; age, 45–79y) who participated in functional performance assessments (timed 20-m walk and chair stand test) at baseline and 1-year follow-up.Interventions: Not applicable.Main Outcome Measure: A good 1-year performance outcome (separately defined for walk time and chair stand measures) was improvement from baseline quintile or maintenance in the best quintile.
Results: Almost 2 in 5 persons with radiographic knee OA improved or maintained high performance at 1 year. Physical activity measured by the Physical Activity Scale for the Elderly (PASE) was significantly associated with good walk rate and chair stand outcomes (odds ratio per 40 units PASE [95% confidence interval]=1.13 [1.13, 1.17] and 1.10 [1.05, 1.15], respectively), as were participation in sports/recreational activities (1.45 [1.23, 1.71] and 1.29 [1.09, 1.51], respectively) and lifestyle activities (1.11 [1.06, 1.16] and 1.09 [1.04, 1.14], respectively). An independent protective relationship for these physical activity measures approached significance after adjusting for sociodemographic and health factors. Older adults reported the least baseline physical activity and least frequent good 1-year outcomes.
Conclusions: These findings support public health recommendations to be physically active in order to preserve function for persons with knee OA. Physical activity messages should specifically target older adults whose low activity levels may jeopardize their ability to maintain functional performance.
Dr. Joshua Brooks
Chiropractor Fairfax VA 22031
Friday, May 7, 2010
Rehab Study for Low Back Pain
Rehabilitation of a Patient with Functional Instability Associated with Failed Back Surgery,
The Journal of the American Chiropractic Association, Dec 2004 by Adams, Vincent
123456Next ..Abstract
Objective: A report of a case of a low-tech non-dynamometric functional exercise program in the rehabilitation of a functionally unstable lower back, associated with failed back surgery.
Clinical Features: A 41-year-old female presented to a chiropractic office with severe lower-back pain, with radiation down the left leg to the calf. Seven months prior, she had an L5-S1 discectomy. Two months after the surgery, her pain in the lower back and leg returned. An MRI 6 months after the surgery showed no evidence of a recurrent disc herniation, but revealed a small image enhancement along the, posterior annulus adjacent to the right S1 nerve root, consistent with post-operative change. Plain film radiography was unremarkable.
Most Recent Health Care Articles Post-Healthcare Reform: Companies Are Already Thinking About Dumping Worker...Tenet Hospital Chain Gets More Buck For the Bang By Milking Patients and Payers
Defensive Medicine vs. Cost Consciousness: How Doctors Actually Make Decisions
Former HCA CEO Rick Scott: Bad News for Florida Healthcare If He Becomes...
Overburdened Health IT Agency Adds Another Big Project: Enrollment in...
Intervention and Outcome: The home-based therapeutic techniques used in this case were based on the patient's weaknesses demonstrated on a functional evaluation. This evaluation consisted of 4 functional tests, including the repetitive squat, Sorenson static back endurance, repetitive sit-up, and the repetitive arch-up tests. The exercises were performed over a 6-week period, and resulted in a decrease in both pain and functional disability based on visual analog scale, pain diagrams, and the Oswestry low-back pain questionnaire.
Conclusion: A home-based exercise program proved very effective in decreasing this patient's functional disability level, but was ineffective in reducing pain levels. Further investigation of chiropractic management of such cases is warranted.
Key Words or Phrases: functional instability, rehabilitation, failed back surgery
Dr. Joshua Brooks
Chiropractor Fairfax VA
The Journal of the American Chiropractic Association, Dec 2004 by Adams, Vincent
123456Next ..Abstract
Objective: A report of a case of a low-tech non-dynamometric functional exercise program in the rehabilitation of a functionally unstable lower back, associated with failed back surgery.
Clinical Features: A 41-year-old female presented to a chiropractic office with severe lower-back pain, with radiation down the left leg to the calf. Seven months prior, she had an L5-S1 discectomy. Two months after the surgery, her pain in the lower back and leg returned. An MRI 6 months after the surgery showed no evidence of a recurrent disc herniation, but revealed a small image enhancement along the, posterior annulus adjacent to the right S1 nerve root, consistent with post-operative change. Plain film radiography was unremarkable.
Most Recent Health Care Articles Post-Healthcare Reform: Companies Are Already Thinking About Dumping Worker...Tenet Hospital Chain Gets More Buck For the Bang By Milking Patients and Payers
Defensive Medicine vs. Cost Consciousness: How Doctors Actually Make Decisions
Former HCA CEO Rick Scott: Bad News for Florida Healthcare If He Becomes...
Overburdened Health IT Agency Adds Another Big Project: Enrollment in...
Intervention and Outcome: The home-based therapeutic techniques used in this case were based on the patient's weaknesses demonstrated on a functional evaluation. This evaluation consisted of 4 functional tests, including the repetitive squat, Sorenson static back endurance, repetitive sit-up, and the repetitive arch-up tests. The exercises were performed over a 6-week period, and resulted in a decrease in both pain and functional disability based on visual analog scale, pain diagrams, and the Oswestry low-back pain questionnaire.
Conclusion: A home-based exercise program proved very effective in decreasing this patient's functional disability level, but was ineffective in reducing pain levels. Further investigation of chiropractic management of such cases is warranted.
Key Words or Phrases: functional instability, rehabilitation, failed back surgery
Dr. Joshua Brooks
Chiropractor Fairfax VA
Wednesday, April 14, 2010
Treatment for Arthritis
Another great article from ACA today...
Don't Take Arthritis Lying Down
Years ago, doctors hardly ever told rheumatoid arthritis patients to "go take a hike" or "go for a swim." Arthritis was considered an inherent part of the aging process and a signal to a patient that it's time to slow down. But not so anymore. Recent research and clinical findings show that there is much more to life for arthritis patients than the traditional recommendation of bed rest and drug therapy.
What Is Rheumatoid Arthritis?
The word "arthritis" means "joint inflammation" and is often used in reference to rheumatic diseases. Rheumatic diseases include more than 100 conditions, including gout, fibromyalgia, osteoarthritis, psoriatic arthritis, and many more. Rheumatoid arthritis is also a rheumatic diseases, affecting about 1 percent of the U.S. population (about 2.1 million people.)1 Although rheumatoid arthritis often begins in middle age and is more frequent in the older generation, it can also start at a young age.
Rheumatoid arthritis causes pain, swelling, stiffness, and loss of function in the joints. Several features distinguish it from other kinds of arthritis:
-Tender, warm, and swollen joints.
-Fatigue, sometimes fever, and a general sense of not feeling well.
-Pain and stiffness lasts for more than 30 minutes after a long rest.
-The condition is symmetrical. If one hand is affected, the other one is, too.
-The wrist and finger joints closest to the hand are most frequently affected. Neck, shoulder, elbow, hip, knee, ankle, and feet joints can also be affected.
-The disease can last for years and can affect other parts of the body, not only the joints.2
-Rheumatoid arthritis is highly individual. Some people suffer from mild arthritis that lasts from a few months to a few years and then goes away. Mild or moderate arthritis have periods of worsening symptoms (flares) and periods of remissions, when the patient feels better. People with severe arthritis feel pain most of the time. The pain lasts for many years and can cause serious joint damage and disability.
Should Arthritis Patients Exercise?
Exercise is critical in successful arthritis management. It helps maintain healthy and strong muscles, joint mobility, flexibility, endurance, and helps control weight. Rest, on the other hand, helps to decrease active joint inflammation, pain, and fatigue. For best results, arthritis patients need a good balance between the two: more rest during the active phase of arthritis, and more exercise during remission.2 During acute systematic flares or local joint flares, patients should put joints gently through their full range of motion once a day, with periods of rest. To see how much rest is best during flares, patients should talk to their health care providers.3
The following exercises are most frequently recommended for patients with arthritis:*
Type of Exercise Benefits Frequency of Exercise
Range-of-motion exercises, e.g. stretching and dance Help maintain normal joint movement and increase joint flexibility. Can be done daily and should be done at least every other day.
Strengthening exercises, e.g. weight lifting Help improve muscle strength, which is important to support and protect joints affected by arthritis. Should be done every other day, unless pain and swelling are severe.
Aerobic or endurance exercises, e.g. walking, bicycle riding, and swimming Help improve the cardiovascular system and muscle tone and control weight. Swimming is especially valuable because of its minimal risk of stress injuries and low impact on the body. Should be done for 20 to 30 minutes three times a week unless pain and swelling are severe.
Range-of-motion exercises, e.g. stretching and dance Help maintain normal joint movement and increase joint flexibility. Can be done daily and should be done at least every other day. Strengthening exercises, e.g. weight lifting Help improve muscle strength, which is important to support and protect joints affected by arthritis. Should be done every other day, unless pain and swelling are severe. Aerobic or endurance exercises, e.g. walking, bicycle riding, and swimming Help improve the cardiovascular system and muscle tone and control weight. Swimming is especially valuable because of its minimal risk of stress injuries and low impact on the body. Should be done for 20 to 30 minutes three times a week unless pain and swelling are severe.
* Adapted from Questions and Answers about Arthritis and Exercise.3
If patients experience
Unusual or persistent fatigue,
Increased weakness,
Decreased range of motion,
Increased joint swelling, or
Pain that lasts more than one hour after exercising,
they need to talk to their health care provider.3 Doctors of chiropractic will help arthritis patients develop or adjust their exercise programs to achieve maximum health benefits with minimal discomfort and will identify the activities that are off limits for this particular arthritis patient.
Nutrition for the Rheumatoid Arthritis Patient
Arthritis medications help suppress the immune system and slow the progression of the disease. But for those who prefer an alternative approach, nutrition may provide complementary support. Some evidence shows that nutrition can play a role in controlling the inflammation, and possibly also in slowing the progression of rheumatoid arthritis.
Some foods and nutritional supplements can be helpful in managing arthritis:
Fatty-acid supplements: eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA), and gamma linolenic acid (GLA). Several studies point to the effectiveness of these fatty acid supplements in reducing joint pain and swelling, and lessening reliance on corticosteroids.4,5
Deep-sea fish, such as salmon, tuna, herring, and halibut, are sources of EPA and DHA. GLA is found in very few food sources, such as black currants and borage seed.
Turmeric, a spice that's used to make curry dishes, may also be helpful. A 95 percent curcuminoid extract has been shown to significantly inhibit the inflammatory cascade and provide relief of joint inflammation and pain.
Ginger extract has been shown to be beneficial in terms of inflammation.
Nettle leaf extract may inhibit some inflammatory pathways.
A vegetarian or low-allergen diet can help with the management of rheumatoid arthritis as well.
The benefits and risks of most of these agents are being researched. Before taking any dietary supplement, especially if you are using medication to control your condition, consult with your health care provider.
What Can Your Doctor of Chiropractic Do?
If you suffer from rheumatoid arthritis, your doctor of chiropractic can help you plan an individualized exercise program that will:
Help you restore the lost range of motion to your joints.
Improve your flexibility and endurance.
Increase your muscle tone and strength.
Doctors of chiropractic can also give you nutrition and supplementation advice that can be helpful in controlling and reducing joint inflammation.

Chiropractor Fairfax, VA 22031
Don't Take Arthritis Lying Down
Years ago, doctors hardly ever told rheumatoid arthritis patients to "go take a hike" or "go for a swim." Arthritis was considered an inherent part of the aging process and a signal to a patient that it's time to slow down. But not so anymore. Recent research and clinical findings show that there is much more to life for arthritis patients than the traditional recommendation of bed rest and drug therapy.
What Is Rheumatoid Arthritis?
The word "arthritis" means "joint inflammation" and is often used in reference to rheumatic diseases. Rheumatic diseases include more than 100 conditions, including gout, fibromyalgia, osteoarthritis, psoriatic arthritis, and many more. Rheumatoid arthritis is also a rheumatic diseases, affecting about 1 percent of the U.S. population (about 2.1 million people.)1 Although rheumatoid arthritis often begins in middle age and is more frequent in the older generation, it can also start at a young age.
Rheumatoid arthritis causes pain, swelling, stiffness, and loss of function in the joints. Several features distinguish it from other kinds of arthritis:
-Tender, warm, and swollen joints.
-Fatigue, sometimes fever, and a general sense of not feeling well.
-Pain and stiffness lasts for more than 30 minutes after a long rest.
-The condition is symmetrical. If one hand is affected, the other one is, too.
-The wrist and finger joints closest to the hand are most frequently affected. Neck, shoulder, elbow, hip, knee, ankle, and feet joints can also be affected.
-The disease can last for years and can affect other parts of the body, not only the joints.2
-Rheumatoid arthritis is highly individual. Some people suffer from mild arthritis that lasts from a few months to a few years and then goes away. Mild or moderate arthritis have periods of worsening symptoms (flares) and periods of remissions, when the patient feels better. People with severe arthritis feel pain most of the time. The pain lasts for many years and can cause serious joint damage and disability.
Should Arthritis Patients Exercise?
Exercise is critical in successful arthritis management. It helps maintain healthy and strong muscles, joint mobility, flexibility, endurance, and helps control weight. Rest, on the other hand, helps to decrease active joint inflammation, pain, and fatigue. For best results, arthritis patients need a good balance between the two: more rest during the active phase of arthritis, and more exercise during remission.2 During acute systematic flares or local joint flares, patients should put joints gently through their full range of motion once a day, with periods of rest. To see how much rest is best during flares, patients should talk to their health care providers.3
The following exercises are most frequently recommended for patients with arthritis:*
Type of Exercise Benefits Frequency of Exercise
Range-of-motion exercises, e.g. stretching and dance Help maintain normal joint movement and increase joint flexibility. Can be done daily and should be done at least every other day.
Strengthening exercises, e.g. weight lifting Help improve muscle strength, which is important to support and protect joints affected by arthritis. Should be done every other day, unless pain and swelling are severe.
Aerobic or endurance exercises, e.g. walking, bicycle riding, and swimming Help improve the cardiovascular system and muscle tone and control weight. Swimming is especially valuable because of its minimal risk of stress injuries and low impact on the body. Should be done for 20 to 30 minutes three times a week unless pain and swelling are severe.
Range-of-motion exercises, e.g. stretching and dance Help maintain normal joint movement and increase joint flexibility. Can be done daily and should be done at least every other day. Strengthening exercises, e.g. weight lifting Help improve muscle strength, which is important to support and protect joints affected by arthritis. Should be done every other day, unless pain and swelling are severe. Aerobic or endurance exercises, e.g. walking, bicycle riding, and swimming Help improve the cardiovascular system and muscle tone and control weight. Swimming is especially valuable because of its minimal risk of stress injuries and low impact on the body. Should be done for 20 to 30 minutes three times a week unless pain and swelling are severe.
* Adapted from Questions and Answers about Arthritis and Exercise.3
If patients experience
Unusual or persistent fatigue,
Increased weakness,
Decreased range of motion,
Increased joint swelling, or
Pain that lasts more than one hour after exercising,
they need to talk to their health care provider.3 Doctors of chiropractic will help arthritis patients develop or adjust their exercise programs to achieve maximum health benefits with minimal discomfort and will identify the activities that are off limits for this particular arthritis patient.
Nutrition for the Rheumatoid Arthritis Patient
Arthritis medications help suppress the immune system and slow the progression of the disease. But for those who prefer an alternative approach, nutrition may provide complementary support. Some evidence shows that nutrition can play a role in controlling the inflammation, and possibly also in slowing the progression of rheumatoid arthritis.
Some foods and nutritional supplements can be helpful in managing arthritis:
Fatty-acid supplements: eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA), and gamma linolenic acid (GLA). Several studies point to the effectiveness of these fatty acid supplements in reducing joint pain and swelling, and lessening reliance on corticosteroids.4,5
Deep-sea fish, such as salmon, tuna, herring, and halibut, are sources of EPA and DHA. GLA is found in very few food sources, such as black currants and borage seed.
Turmeric, a spice that's used to make curry dishes, may also be helpful. A 95 percent curcuminoid extract has been shown to significantly inhibit the inflammatory cascade and provide relief of joint inflammation and pain.
Ginger extract has been shown to be beneficial in terms of inflammation.
Nettle leaf extract may inhibit some inflammatory pathways.
A vegetarian or low-allergen diet can help with the management of rheumatoid arthritis as well.
The benefits and risks of most of these agents are being researched. Before taking any dietary supplement, especially if you are using medication to control your condition, consult with your health care provider.
What Can Your Doctor of Chiropractic Do?
If you suffer from rheumatoid arthritis, your doctor of chiropractic can help you plan an individualized exercise program that will:
Help you restore the lost range of motion to your joints.
Improve your flexibility and endurance.
Increase your muscle tone and strength.
Doctors of chiropractic can also give you nutrition and supplementation advice that can be helpful in controlling and reducing joint inflammation.

Chiropractor Fairfax, VA 22031
Wednesday, March 31, 2010
Poor posture can lead to poor health
Poor posture can lead to poor health
Prevention and awareness is the best care for health-related problems. One of the easiest and most logical ways to prevent bad posture habits is to think about the consequences.
1. Tension Headaches: Sitting hunched over at your job, most commonly caused by your hands reaching for the keyboard when typing on your computer leads to your shoulders and head slumping forward. This posture tightens the muscles in your neck, upper back and shoulders. After awhile, the tightness causes nerve irritations and muscle spasms which restrict proper flow of blood to the back of your head. This leads to tension headaches.
2. Diminished Breathing: Poor posture can lead to severe kyphosis (hunched back) causing the torso collapse leading to breathing difficulties. Rounded shoulders and overly bent or imbalanced spine restrict the expansion of the rib cage, which restricts the rise and fall of the breathing diaphragm. Reduced rib and spinal mobility will affect the normal breathing movement. If the diaphragm can't rise, it won't be able to draw in as much oxygen during inhalation.
3. Fatigue: Fatigue is one of the most common causes of bad posture. Tired and tight muscles cannot support the skeleton as they are designed to do. Your muscles have to work extra hard just to hold you up if you have poor posture, leaving you without energy. Lack of adequate muscle flexibility and strength, abnormal joint motion in the spine and other body regions will lead to overall muscle fatigue.
4. Make you look older: Never underestimate the beauty and health benefits of good posture. Often poor posture is just a bad habit that is easily corrected. Poor posture not only makes you look older, but could be the first step toward dowager’s hump, double chin, potbelly, and swayback as well as some internal problems too. When a person is hunched over or not standing straight that person may be perceived as older than they actually are. Good posture is not only beneficial to your body; it also makes you look taller and slimmer. What's more, good posture can convey self-confidence, which may just be the best accessory you can have.
5. Back pain: Most common consequence of poor posture, due to muscle strain, especially lower back pain. The back muscles, ligaments, and discs are under extra stress when the spine is not in proper alignment. Strong muscles help keep the spine in proper alignment and prevent back pain. Strong muscles also prevent the spine from extending beyond its normal range of motion, which is essential to protecting the ligaments and disks from injury.
Source: T. Moses Public Relations and Consulting, http://tmosespublicrelations.com
Prevention and awareness is the best care for health-related problems. One of the easiest and most logical ways to prevent bad posture habits is to think about the consequences.
1. Tension Headaches: Sitting hunched over at your job, most commonly caused by your hands reaching for the keyboard when typing on your computer leads to your shoulders and head slumping forward. This posture tightens the muscles in your neck, upper back and shoulders. After awhile, the tightness causes nerve irritations and muscle spasms which restrict proper flow of blood to the back of your head. This leads to tension headaches.
2. Diminished Breathing: Poor posture can lead to severe kyphosis (hunched back) causing the torso collapse leading to breathing difficulties. Rounded shoulders and overly bent or imbalanced spine restrict the expansion of the rib cage, which restricts the rise and fall of the breathing diaphragm. Reduced rib and spinal mobility will affect the normal breathing movement. If the diaphragm can't rise, it won't be able to draw in as much oxygen during inhalation.
3. Fatigue: Fatigue is one of the most common causes of bad posture. Tired and tight muscles cannot support the skeleton as they are designed to do. Your muscles have to work extra hard just to hold you up if you have poor posture, leaving you without energy. Lack of adequate muscle flexibility and strength, abnormal joint motion in the spine and other body regions will lead to overall muscle fatigue.
4. Make you look older: Never underestimate the beauty and health benefits of good posture. Often poor posture is just a bad habit that is easily corrected. Poor posture not only makes you look older, but could be the first step toward dowager’s hump, double chin, potbelly, and swayback as well as some internal problems too. When a person is hunched over or not standing straight that person may be perceived as older than they actually are. Good posture is not only beneficial to your body; it also makes you look taller and slimmer. What's more, good posture can convey self-confidence, which may just be the best accessory you can have.
5. Back pain: Most common consequence of poor posture, due to muscle strain, especially lower back pain. The back muscles, ligaments, and discs are under extra stress when the spine is not in proper alignment. Strong muscles help keep the spine in proper alignment and prevent back pain. Strong muscles also prevent the spine from extending beyond its normal range of motion, which is essential to protecting the ligaments and disks from injury.
Source: T. Moses Public Relations and Consulting, http://tmosespublicrelations.com
Friday, March 19, 2010
Spinal Decompression Therapy, Fairfax VA
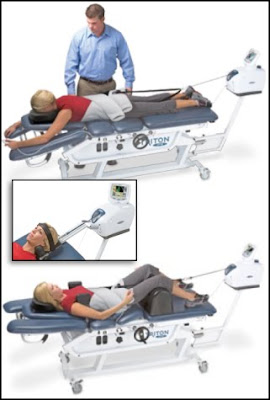
Spinal Decompression Therapy, Fairfax VA
Spinal Decompression Therapy is a safe, effective, revolutional non-surgical treatment for a variety of low back and neck conditions. This therapy's primary benefit works by restoring proper function to an injured disc. It is done by producing a controlled, mechanical traction on the spine using our Triton DTS Decompression Table. During the pull phase, injured discs are gently stretched apart, producing a suction force inside the disc. This draws disc bulges and herniations back into the center of the disc along with oxygen, water, nutrients, and other healing substances. The end result is a strong, healthy, properly functioning disc in a high percentage of patients.
Comfort is Our Top Priority
We want patient visits to be enjoyable and successful! Treatments are short in duration and administered while the patient is fully clothed. Most patients undergoing this treatment report improvements and a reduction in their pain after only a few sessions. DTS Therapy gently stretches the spine, relieving pressure from the discs, joints and muscular tissues.
Patient comfort and safety are of primary importance during DTS Spinal Decompression Therapy. There are several positioning options, so you will be able to rehabilitate the discs and spine while remaining comfortable. During DTS Therapy, you'll experience several cycles of stretch and relaxation, which gently graduate to a peak over a period of several minutes.
Therapy sessions typically last less than 20 minutes and most patients feel pain relief with as few as 6-10 treatments. It is important to remember, however, that pain reduction does not necessarily mean that your discs and spine are healed, so it is critical that patients stick with the treatment protocol prescribed by their practitioners in order to achieve the full value of DTS Therapy.
DTS Spinal Decompression Therapy is a pain-free alternative that has shown a very high rate of success at reducing or even eliminating back and neck pain.. Our office is dedicated to offering the latest, state-of-the-art therapies for lower back pain, sciatica pain relief, pinched nerve, neck pain relief, and bulging or degenerative disc diseases. We believe DTS Spinal Decompression Therapy is one of the most advanced, non-surgical and pain-free alternative.
Spinal Decompression Therapy is an Effective Treatment for:
Herniated Disc
Degenerative Disc
Facet Syndrome
Sciatica
Post-Surgical Patients
Spinal Stenosis
For more information, please visit www.dtstherapy.com or consult with one of our health care professionals!
Chiropractor
Fairfax, VA 22031
Bike Fit using Video Motion Analysis Dartfish
Bike Fit using Video Motion Analysis Dartfish
Many injuries that occur as a result of ridding a bike can be traced back to poor bike positioning.
The first step to correcting a problem or gaining some watts on the bike is with a proper bike fit. There are many schools of thought and methods but I feel that SICI ( Serotta International Cycling Institute) has the best methods, training staff and the ability to know its reproducible. Using Video to analyze motion has been around for years the first exposure I had was working with Dr. Robert Roe a chiropractor that had worked at the Olympic training center in Colorado in the early 90 using a much more cumbersome and primitive form of analysis. At that time we were using it to evaluate work loads on patients. Now I have been using Dart fish to analyze bio-mechanics of all types of athletes. At SICI we trained using there fitting principles and High Def cameras to evaluate motion down to the smallest detail. It is a more dynamic fitting process that can breakdown movement to a much higher degree. When you add power and HR data things get even more interesting. The amount of information and precision is really remarkable. I have added a video of a fit I did in Northern Virginia of a Pro cyclist that is having a few problems even after several Bike fits by other professionals.
This is an example of a marker that was placed on his right leg that is short when compared to the left and is not tracking properly. The patient feels like his right leg is wobbly and dives in medialy on the power stoke. He notes hitting the top tube. I will also let you know that after the exam I also found very specific weak core strength that needed to be address. Using this software and combining that my physical exam finding I am able to find a new starting point to make small adjustments until the correct fit is obtained.
Dr. Rick Rosa
Fairfax & Alexandria VA
703-876-5600
Many injuries that occur as a result of ridding a bike can be traced back to poor bike positioning.
The first step to correcting a problem or gaining some watts on the bike is with a proper bike fit. There are many schools of thought and methods but I feel that SICI ( Serotta International Cycling Institute) has the best methods, training staff and the ability to know its reproducible. Using Video to analyze motion has been around for years the first exposure I had was working with Dr. Robert Roe a chiropractor that had worked at the Olympic training center in Colorado in the early 90 using a much more cumbersome and primitive form of analysis. At that time we were using it to evaluate work loads on patients. Now I have been using Dart fish to analyze bio-mechanics of all types of athletes. At SICI we trained using there fitting principles and High Def cameras to evaluate motion down to the smallest detail. It is a more dynamic fitting process that can breakdown movement to a much higher degree. When you add power and HR data things get even more interesting. The amount of information and precision is really remarkable. I have added a video of a fit I did in Northern Virginia of a Pro cyclist that is having a few problems even after several Bike fits by other professionals.
This is an example of a marker that was placed on his right leg that is short when compared to the left and is not tracking properly. The patient feels like his right leg is wobbly and dives in medialy on the power stoke. He notes hitting the top tube. I will also let you know that after the exam I also found very specific weak core strength that needed to be address. Using this software and combining that my physical exam finding I am able to find a new starting point to make small adjustments until the correct fit is obtained.
Dr. Rick Rosa
Fairfax & Alexandria VA
703-876-5600
Thursday, March 18, 2010
Study shows that Cold Laser Therapy helps Chronic Neck Pain Sufferers
Study shows that Cold Laser Therapy helps Chronic Neck Pain Sufferers
A new Australian study appeared in the journal Lancet shows that using cold laser therapy to treat chronic neck pain can be very effective.
Low-level laser therapy, also known as LLLT involves using a laser's light to stimulate tissue repair and ease pain. Lead researcher Roberta Chow of the Brain and Mind Research Institute at Australia's University of Sydney carried out an overview of 16 randomized trials that put this increasingly popular procedure to the test. 820patients were enrolled in the trials and divided into two groups: one that received either the therapy or other one that received a dummy treatment.
In five trials, the researchers found that patients given LLLT were around four times more likely to have reduced pain compared with a placebo. In the 11 other trials, for which there was a detailed analysis of pain symptoms, LLLT patients reported reductions of chronic pain by around 20 points on a scale of 100 points. The pain reduction continued for up to 22 weeks.
LLLT compares favorably with other drugs and remedies for effectiveness and its side-effects are mild, says the study. The researchers further suggested that low level laser therapy be used in combination with an exercise program for neck pain as well.
Original article: Chow RT, Johnson MI, Lopes-Martins RA, Bjordal JM. “Efficacy of low-level laser therapy in the management of neck pain: a systematic review and meta-analysis of randomised placebo or active-treatment controlled trials.” Lancet. 2009 Dec 5;374(9705):1897-908.
Rick Rosa,D.C.,D.A.A.P.M
2750 Prosperity Ave, Suite #550, Fairfax VA
www.rosachiropracticfairfax.com/
A new Australian study appeared in the journal Lancet shows that using cold laser therapy to treat chronic neck pain can be very effective.
Low-level laser therapy, also known as LLLT involves using a laser's light to stimulate tissue repair and ease pain. Lead researcher Roberta Chow of the Brain and Mind Research Institute at Australia's University of Sydney carried out an overview of 16 randomized trials that put this increasingly popular procedure to the test. 820patients were enrolled in the trials and divided into two groups: one that received either the therapy or other one that received a dummy treatment.
In five trials, the researchers found that patients given LLLT were around four times more likely to have reduced pain compared with a placebo. In the 11 other trials, for which there was a detailed analysis of pain symptoms, LLLT patients reported reductions of chronic pain by around 20 points on a scale of 100 points. The pain reduction continued for up to 22 weeks.
LLLT compares favorably with other drugs and remedies for effectiveness and its side-effects are mild, says the study. The researchers further suggested that low level laser therapy be used in combination with an exercise program for neck pain as well.
Original article: Chow RT, Johnson MI, Lopes-Martins RA, Bjordal JM. “Efficacy of low-level laser therapy in the management of neck pain: a systematic review and meta-analysis of randomised placebo or active-treatment controlled trials.” Lancet. 2009 Dec 5;374(9705):1897-908.
Rick Rosa,D.C.,D.A.A.P.M
2750 Prosperity Ave, Suite #550, Fairfax VA
www.rosachiropracticfairfax.com/
Subscribe to:
Posts (Atom)
